Brian Maranan Pineda for NRDC
Human Health
Overview
At the forefront of our collective fight for a just, sustainable, and socially equitable world is human health. And our health is intimately tied to the air we breathe, water we drink, food we eat, products we use, and places where we live, learn, work, and play. We must protect the health of our communities and ensure that all people have a meaningful voice in their well-being. Our future—and our resilience—depends on our ability to deliver a just, clean, and healthy environment for all.
Solutions
Throughout our policy, advocacy, and coalition-building work, we’re focused on intersectional strategies in order to improve public health outcomes, particularly for the populations facing the greatest health disparities. Here are our current priorities:
Build power for the grassroots environmental justice movement
Low-income residents and communities of color are disproportionately targeted within our social systems, including health care, transportation, judicial, and industrial systems. The injustices add up and compound each other, leading to less opportunity and increased health impacts such as higher levels of mental and physical stress; higher exposure to pollutants; and shortened longevity, among many other worsened health outcomes. NRDC is supporting communities in co-creating their future and defining their own solutions. We are working to ensure that these communities not only have a seat at the table but are leading how climate and public policies are developed. Their needs and recommendations must be well incorporated into everything from infrastructure planning to the building of the clean energy workforce.
Reduce smog, soot, toxic, and indoor air pollution
In the United States, people of color are 1.5 times more likely than white people to live in areas with poor air quality. Historically, racist zoning policies and the discriminatory lending practices known as redlining have combined to keep polluting industries and car-choked highways away from white neighborhoods and have turned communities of color—especially poor and working-class communities of color—into sacrifice zones where residents are forced to breathe dirty air and suffer the many health problems associated with it. The most effective way to control air pollution—which both worsens climate change and is worsened by climate change—is to reduce our burning of fossil fuels (coal, oil, and gas), and that encompasses solutions we’ve been championing in the United States and through partnerships with clean air advocates in India and China. By reforming discriminatory land use patterns, transitioning to renewable energy sources (such as wind and solar power), maximizing fuel efficiency in our vehicles, replacing more of our gasoline-powered cars and trucks with electric versions, and shifting to technologies such as heat pumps and induction stoves to decarbonize our homes, we'll be limiting air pollution at its many sources while also improving the health of millions of people.
Did You Know?
Instead of ensuring that the most vulnerable in our society have access to essential utility services, such as water and electricity, many states allow utilities to disconnect households when they cannot afford their monthly bills. Late fees and other punitive charges compound the problem by increasing the amount that struggling households must pay to access, maintain, or restore power and water service. These disconnections disproportionately harm people of color and the elderly and result in serious health implications.
Secure safe, sufficient, and affordable drinking water
Access to affordable and safe drinking water, especially for marginalized communities, is a life-or-death matter. That’s why we’re pushing to immediately reform our nation’s drinking water infrastructure, which includes replacing millions of toxic lead service lines bringing water into homes and addressing disparities in state infrastructure that increases the health threats from bacterial contamination and improper disinfection. We also are working to secure health-protective drinking water standards for PFAS, perchlorate, and hexavalent chromium. In addition, we’re ensuring that household income does not limit access to this basic human right by advocating for utility shutoff moratoriums alongside the expansion of low-income utility assistance programs. Finally, we are championing new standards that ensure there’s enough water to go around as inefficiencies in our infrastructure and increasing drought put pressure on drinking water supplies.
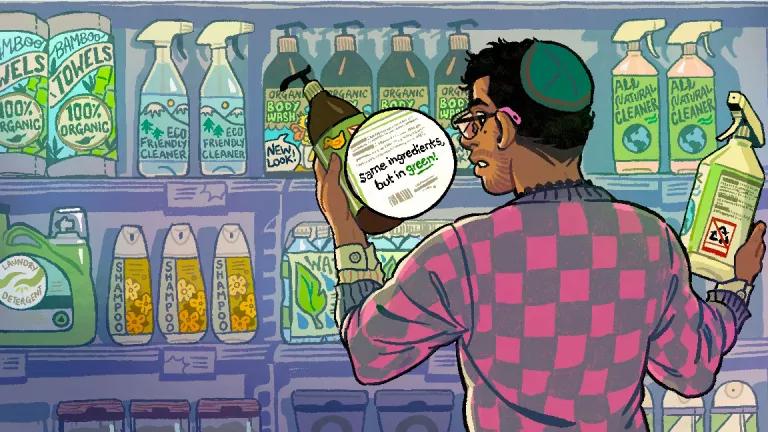
Remove toxic chemicals from household products and building materials
Many chemicals that are widely used in consumer products and industrial processes are harmful to human health, from PFAS (found in everything from clothing to drinking water to food packaging) to flame retardants (used in furniture, baby products, electronics, and building insulation). To ensure a healthy future for our children and communities, we must address the sources of these harmful chemicals across their life cycle, from production through disposal. We advocate for science-based policies, stronger regulations, and marketplace reforms to phase them out, in partnership with the frontline communities disproportionately exposed to toxic chemicals.
Transform agriculture and food systems
Farm- and food workers are facing disproportionate health risks, low-income communities are grappling with increasing food insecurity, and our infrastructure does not adequately sustain regional food systems. We advocate for reforms to our conventional growing systems, including those that increase food sovereignty and decrease reliance on synthetic fertilizers, pesticides, and the “factory farms” that contaminate water, air, and soil and fuel antibiotic resistance—a serious health threat to residents of surrounding communities. We also work to strengthen worker safety standards for the food sector, where increasing exposure to extreme heat, wildfire smoke, and other climate impacts demands immediate, systemic changes.
“Supporting clean energy saves tens of thousands of lives today and billions of dollars in health-care costs by reducing air pollution and limiting the worst effects of climate change.”
Kim Knowlton, senior scientist, Science Office
Progress
- Recognizing the need to combat dangerous air pollution, the Indian government launched the National Clean Air Programme (NCAP) in 2019 to reduce outdoor air pollution in more than a hundred of the country’s most polluted cities. In 2022, it is in the process of scaling up the NCAP to a national mission, “Clean Air for All,” and has committed to enhancing its goal of a 20 to 30 percent cut in air pollution levels (from 2017 levels) by 2024.
- California launched a new Farm to School program in 2021 that commits to giving school districts extra resources when they purchase from local growers who are using organic and other climate-smart systems and practices. Federal lawmakers are considering adopting this approach in the 2023 Farm Bill. This would increase production of healthy food grown without toxic pesticides and under climate-friendly farming practices.
- The U.S. Department of Health and Human Services now has an Office of Climate Change and Health Equity (OCCHE) for the first time in its history. OCCHE’s priorities include, among other things, addressing health disparities exacerbated by climate impacts and fostering innovation in adaptation for disadvantaged communities.
- NRDC experts first exposed the dangers of pesticides used in certain collars intended to protect pets from fleas and ticks in 2000. A follow-up report nine years later showed that residue from the chemicals in those collars can be found on pets’ fur at levels that are dangerous for kids. Our analysis and advocacy led to limited action from the U.S. Environmental Protection Agency in 2014; then finally, after ongoing pressure from NRDC, the agency announced in 2022 that it was granting our petition to ban collars with tetrachlorvinphos (TCVP) and would begin the regulatory process to take them off the market.
More Ways to Make an Impact
Latest News & Resources
Millions of Americans drink tap water served by toxic lead pipes.
Tell the EPA we need safe drinking water!

Tell the EPA we need safe drinking water!
There is no safe level of lead exposure. But millions of old lead pipes contaminate drinking water in homes in every state across the country. We need the EPA to do its part to replace lead pipes equitably and quickly.
View All Issues

Climate Change

Equity & Justice

Human Health